Do You Know The #1 Reason Why Your Claims Get Denied? Eligibility Errors
There are $3 trillion medical claims that are submitted annually.$262 billion of those are initially denied.
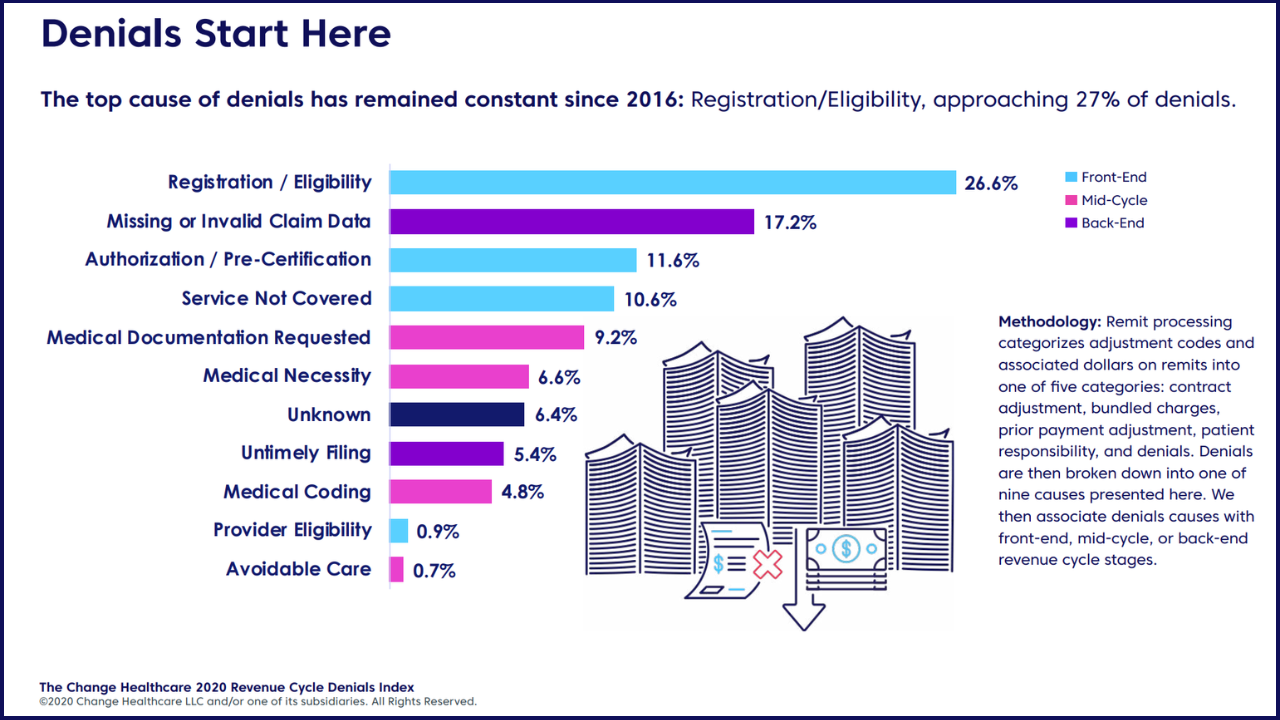
Do you know what the top reason why claims are denied? Coming in at #1 is eligibility errors.
The majority of eligibility errors can be prevented by doing comprehensive benefits checks. This is time consuming and involves calling the payer (maybe multiple times) in order to check everything that you need to know before seeing patients.
Here are some tips on how to set up a verification of benefits process at your clinic
1.) How to Handle New Patient Registration
Some clinics book an appointment and then verify benefits. Some clinics verify benefits before putting a patient on the schedule. It doesn’t matter which one you choose. You should choose whichever way is best for your clinic. The most important thing is to stick to a specific process so everyone at the front desk does the same thing and collects the same information from patients. If you can get a copy of their insurance card, it’s always helpful to keep that on file.
2.) Questionnaire
Once you have a certain process on collecting patient information, it’s important to create a template questionnaire for your staff to make sure you are all collecting the same information. We have a blog post on some questions most clinics find helpful.
3.) Use of Portals
Now that you know what questions you need answered, the first step is to figure out if the payer has any portals that feature any information about eligibility. You should use the portal as the first line of defense. Availity is a great resource you can use to collect information like the patient’s deductible, out of pocket max, copay or coinsurance. Sometimes it will give you information on any limitations as well. Answer all the questions you can using the portals and then call the insurance companies to collect the remaining information.
4.) Call
Now that you have a good understanding of the patient’s benefits, it’s time to call the insurance company to ask your remaining questions and have the insurance rep confirm all the questions you were able to answer using the portals
By sticking to a process like this, you’ll be able to avoid all preventable eligibility errors. If you are short staffed or would like to learn more about having One Body help you with your verifications, please fill out the contact form below!
